Does Adult Aquired Flat Feet Always Require Surgery Teatment ?
Overview
Posterior tibial tendon dysfunction is one of several terms to describe a painful, progressive flatfoot deformity in adults. Other terms include posterior tibial tendon insufficiency and adult acquired flatfoot. The term adult acquired flatfoot is more appropriate because it allows a broader recognition of causative factors, not only limited to the posterior tibial tendon, an event where the posterior tibial tendon looses strength and function. The adult acquired flatfoot is a progressive, symptomatic (painful) deformity resulting from gradual stretch (attenuation) of the tibialis posterior tendon as well as the ligaments that support the arch of the foot. 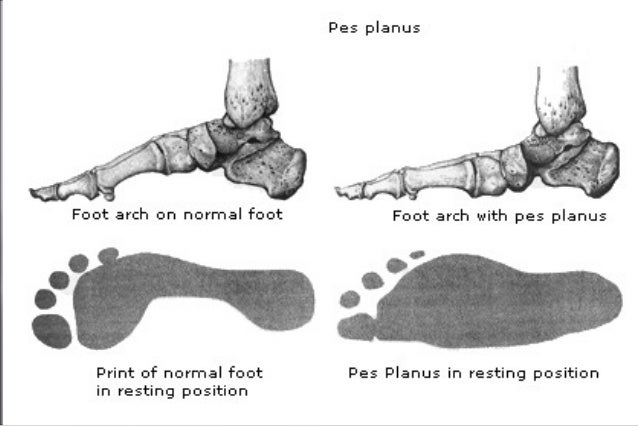
Causes
As discussed above, many different problems can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to support the arch of your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch. An injury to the tendons or ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. Injuries to tendons of the foot can occur either in one instance (traumatically) or with repeated use over time (overuse injury). Regardless of the cause, if tendon function is altered, the forces that are transmitted across joints in the foot are changed and this can lead to increased stress on joint cartilage and ligaments. In addition to tendon and ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. People with diabetes or with nerve problems that limits normal feeling in the feet, can have collapse of the arch or of the entire foot. This type of arch collapse is typically more severe than that seen in patients with normal feeling in their feet. In addition to the ligaments not holding the bones in place, the bones themselves can sometimes fracture and disintegrate without the patient feeling any pain. This may result in a severely deformed foot that is very challenging to correct with surgery. Special shoes or braces are the best method for dealing with this problem.
Symptoms
Pain and swelling around the inside aspect of the ankle initially. Later, the arch of the foot may fall (foot becomes flat), this change leads to walking to become difficult and painful, as well as standing for long periods. As the flat foot becomes established, pain may progress to the outer part of the ankle. Eventually, arthritis may develop.
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise. A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet - the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non surgical Treatment
Icing and anti-inflammatory medications can reduce inflammation and physical therapy can strengthen the tibial tendon. Orthotic inserts that go inside your shoes are a common way to treat and prevent flatfoot pain. Orthotics control the position of the foot and alleviate areas of pressure. In some cases immobilization in a cast or walking boot is necessary to relieve symptoms, and in severe cases surgery may be required to repair tendon damage. 
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.